Benefits of Yoga in Fibromyalgia Patients
Lazaridou A, Buliteanu A, Vijjeswarupa MA, Teodosiadis A, Dorado K, Edwards RE, Schreiber KL, Department of Anesthesiology, Perioperative, and pain medicine, Brigham and Women’s Hospital/Harvard Medical School, Boston, Massachusetts
Ecological Momentary Assessment of the Relationships between Sleep Affliction, Neuroendocrine Response, and Allodynia in Fibromyalgia Patients: The Impact of Daily Yoga Based Exercise (Asana)
Background
- There is growing evidence that alternative therapies such as yoga, exercise and meditation can improve outcomes for patients with chronic pain syndromes, such as Fibromyalgia (FM), which have proven to be notably resistant to conventional pharmacological approaches.
- Fibromyalgia is characterized by persistent, widespread pain, myofascial tenderness, high levels of distress, and dysregulated sleep. It is thought that HPA axis abnormalities may contribute to the pathophysiology of FM*1.
- Previous studies have shown beneficial effects of exercise in FM*2, but it is often difficult for patients to begin regular exercise because of widespread pain.
- Yoga is a holistic practice that combines many of these non-pharmacological therapies, incorporating gentle physical exercise and stretching, breathing techniques, and mindfulness.
- This pilot study investigates the introduction of daily exercise and meditation through participation in a gentle yoga program on sleep, pain, and psychosocial function in FM patients.
Hypothesis
Daily yoga-based exercise and meditation can improve pain and FM symptoms, sleep disturbance and psychosocial function in patients with fibromyalgia.
Methods
After initial screening and enrolment of 38 subjects, 28 patients completed the program (74%), each of whom served as their own control before and after intervention.
Inclusion criteria: age 18–75, FM diagnosis for > 6 months (Wolfe criteria*3), average daily pain score of 4/10 or greater, at least mild degree of sleep disturbance (PSQI score > 5), not currently engaged in rigorous physical exercise routine, stable dose of medications, access to a computer or tablet at home, and proficiency with e-mail.
Visit 1: Informed consent, self-report questionnaires designed to assess pain, sleep quality, and psychosocial function.
Demographics, Health History, Brief Pain Inventory (BPI), PROMIS short forms for anxiety and sleep disturbance, the Pittsburgh Sleep Quality Index (PSQI), a measure of fatigue (VAS 0-10), Pain Catastrophizing Scale (PCS) the FFMQ (Five Facets of Mindfulness Questionnaire), the Perceived Stress Scale (PSS) and Revised Fibromyalgia Impact Questionnaire (FIQR) Quantitative sensory testing (QST): Temporal summation of pinprick pain, temporal summation of leg cuff pain, distraction analgesia, pressure pain threshold, conditioned pain modulation, and cold pain ratings.
Satyananda Yoga Program: Subjects attended a 6-week Satyananda Yoga program specifically adjusted for chronic pain patients.
Each weekly in person session lasted approximately 1.5 hours, including asana, pranayama, yoga nidra, meditation.
Subjects were then sent a daily 30-minute yoga video for practice at home.
Ecologic Momentary Assessment: During 3 weeks (before yoga, week 2 of yoga, and week 6 of yoga) subjects were asked to participate in a more intensive data collection, including:
saliva samples 3x daily to assess cortisol awakening response, upon wakening, actiwatch to assess sleep function, and twice daily completion of electronic symptom diaries (via Redcap) to assess their day-to-day pain experiences, fatigue, anxiety, stress and sleep.
Visit 2: After completing the 6 weeks of daily exercise, subjects underwent the same testing as in Visit 1 (QST and psychosocial variables via questionnaire completion).
Statistics: Paired sample t-test was used to compare pain, FM symptom, and PCS scores between baseline and post-yoga. Independent sample t-test was used to compare groups. Pearson Correlation was calculated to determine association between variables.
Results
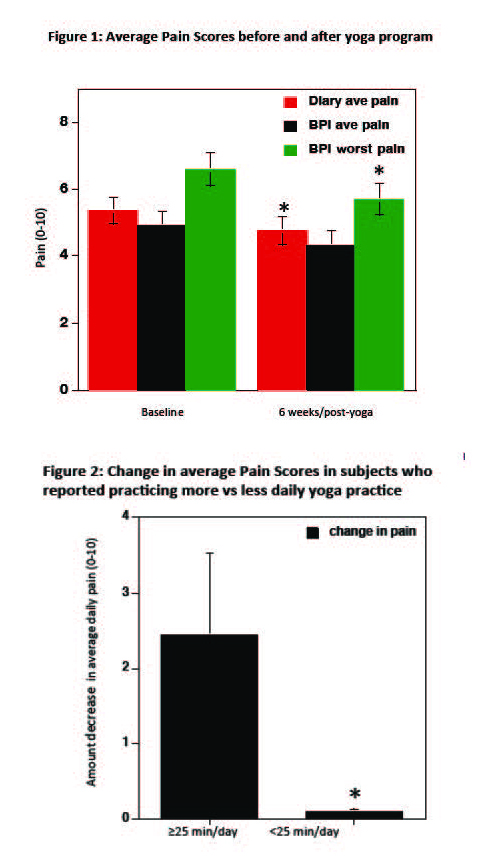
- Average daily pain reported on pain diary significantly decreased between baseline and week 6 of yoga (p=0.042, Figure 1).
- Reported worst (p=0.016), but not average pain (p=0.55) on BPI significantly decreased from baseline to post yoga intervention (Figure 1).
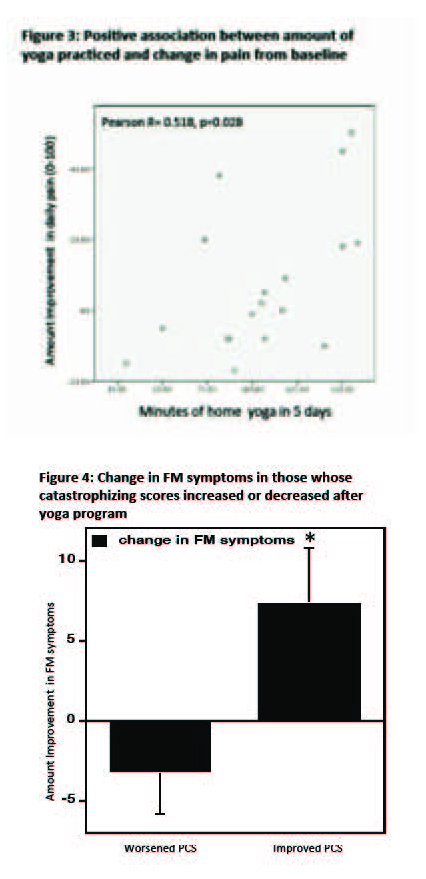
- There was variability among participants in terms of both amount of daily home yoga practised, as well as decrease in pain symptoms. Greater benefit seen in subjects that practised for an average of 25 minutes/day or higher (28% of subjects), compared to those who practised less than 25 minutes/day (72% of subjects) (p=0.023). (Figure 2 and 3)
- Those whose catastrophizing (PCS scores) decreased during the yoga program (57% of subjects) also had greater improvement in fibromyalgia symptoms (p=0.031) (Figure 4).
Discussion
This preliminary analysis of our pilot study on yoga intervention in FM patients suggests that there is a modest overall improvement in reported daily pain on electronic pain diaries, although mixed results on the BPI and FIQR.
•There was substantial variability in adherence to the goal of daily home yoga practice, but those who were able to practise >25 min/day showed greater improvement in their pain.
•The impact of the yoga program on catastrophizing was also variable, but those who improved in terms of catastrophizing also showed decreases in reported FM symptoms.
•Further analysis of the full sample will further investigate the impact of yoga-based exercise on stress responses and sleep, and whether this is related to changes in pain and other symptoms in FM.
•Further analysis will also explore which patient characteristics can predict individuals who will gain most from yoga-based exercise.
References
*1. Riva R, Mork PJ, Westgaard RH, Lundberg U. Comparison of the cortisol awakening response in women with shoulder and neck pain and women with fibromyalgia. Psychoneuroendocrinology. 37(2):299-306 (2012).
*2. Busch AJ, Webber SC, Richards RS, Bidonde J, Schachter CL, Schafer LA, Danyliw A, Sawant A, Dal Bello-Haas V, Rader T, Overend TJ. Resistance exercise training for fibromyalgia. Cochrane Database Syst. Rev. (2013).
*3. Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB: The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 62:600-610 (2010).